“With the largest NCD burden occurring in low- and middle-income countries (LMICs) and leading to and perpetuating poverty, the prevention and control of NCDs is an urgent development issue. The costs to individuals and society of healthcare and loss of income-earners hampers poverty reduction and sustainable development. NCDs constrain the bottom billion in chronic poverty.”
This Wilton Park dialogue will bring together diverse stakeholders from government, health, private sector and other organisations to devise plans and models to unlock the enormous potential of digital health care to facilitate the prevention, treatment and management of NCDs.
The dialogue will take place one year after the publication of the Broadband Commission Working Group on Digital Health report, which highlighted the promise of digital health to address NCDs to accelerate Universal Health Coverage (UHC) in LMICs. It will also follow the United Nations High Level Meeting on UHC in September 2019, with its particular focus on primary healthcare.
Digital health toolkit
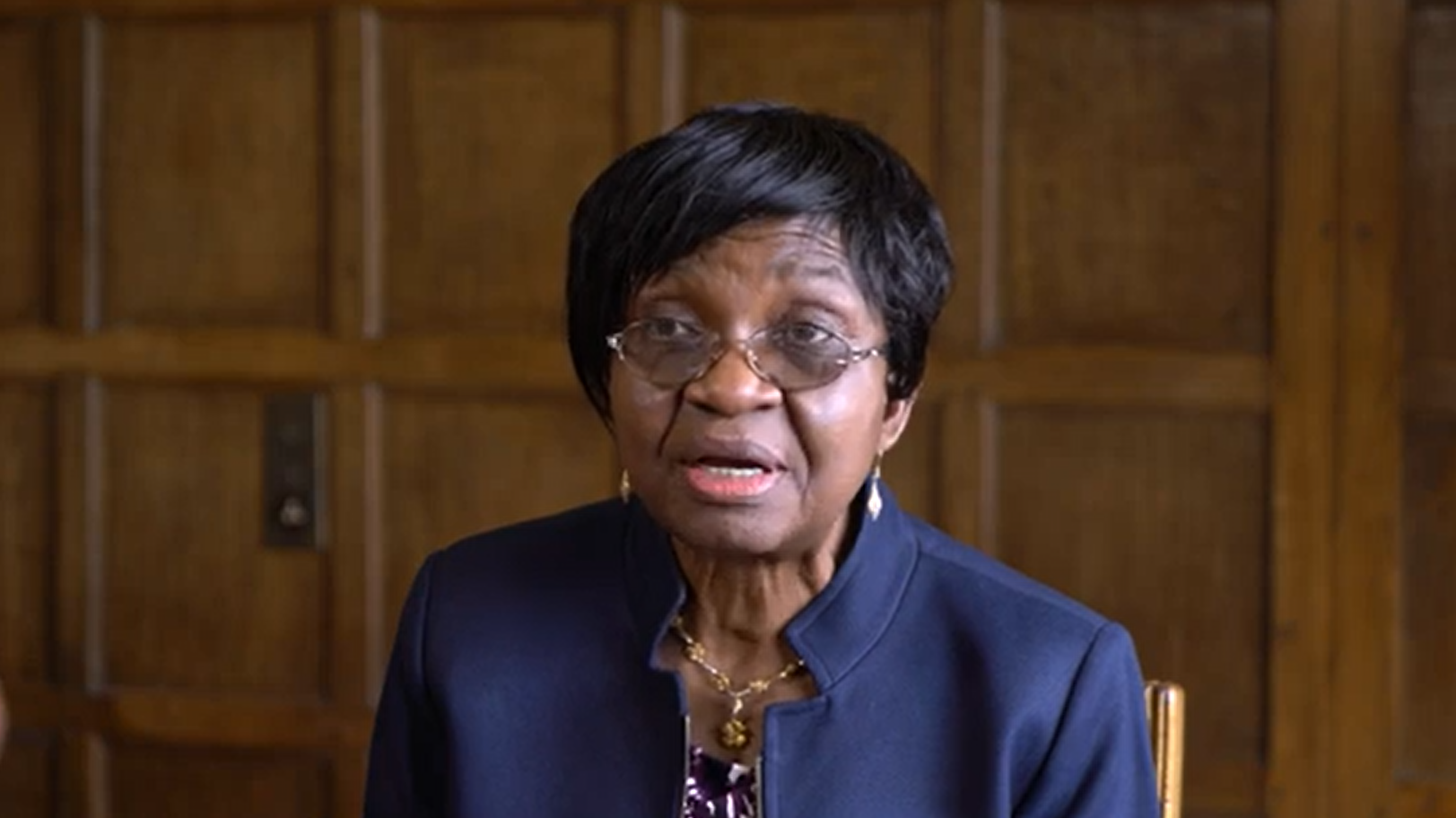
At the dialogue, we interviewed a number of participants asking for their experiences in using digital health to address non-communicable diseases in Low and Middle Income Countries, exploring the potential, the challenges and the opportunities which they had faced.
Please see below the individual interviews: all the interviews can be accessed via this playlist.
Dr Monika Arora, Public Health Foundation of India
Dr Ngo Quang Nguyen, Ministry of Health, Vietnam
Dr David Okello, African Centre for Global Health and Social Transformation
Professor David Peiris, The George Institute for Global Health
Sameer Pujari, World Health Organization
Context
Non-communicable diseases (NCDs) are not a new health challenge. NCDs are becoming an increasing burden for governments of low–and middle–income countries already struggling to improve health outcomes for their populations. More than three quarters (32 million) of all NCD deaths occur in developing countries, and for all regions, except Africa, NCDs are now the leading cause of death. It is projected that by 2030, this will also be the case in Africa.2
The impact of NCDs in LMICs, and particularly through premature deaths (those of working age), is therefore enormous, both causing and perpetuating poverty, while hindering economic development. In fact, NCDs are now considered to be “one of the major challenges for sustainable development in the twenty-first century”3 and are estimated to cause a cumulative global loss of output of $47 trillion between 2011 and 2030.
Despite this global health challenge, funding for tackling NCDs remains low compared to other diseases, attracting just 2% of the funding despite NCDs representing 60% of the disease burden worldwide. Yet even low-cost preventative measures could have a significant impact on future health outcomes. A new approach is therefore needed to combat NCDs: an approach which will transform the way health care is provided and vastly expand access to quality services, as well as promoting effective self-health care among populations.
Without properly addressing NCDs, the goal of Universal Health Coverage (UHC), and the targets of Sustainable Development Goal (SDG) 3, cannot be achieved. This was noted clearly at the UN General Assembly High Level meeting on NCDs in September 2018.
Digital technology, already revolutionising healthcare delivery, offers a way forward. Worldwide, digital tools are leading to better and faster healthcare: healthcare that is more empowering and accessible for patients, more efficient for providers and more cost-effective for health systems. Digital health is potentially the most powerful enabler that LMICs can use to address the growing burden of NCDs and achieve UHC – whether supporting prevention or treatment, management and control.
Despite their potential, the myriad of digital health solutions are often designed and rolled out with a narrow, tactical scope (for example a specific disease, geographic location, or patient (sub)population), and consequently struggle to progress beyond the pilot phase, to become financially viable and integrate into national health policies and systems. There are also a range of challenges to consider, including data privacy, access to digital health for the most vulnerable, or for those in humanitarian settings, or how digital might apply to different demographics, for example it might appeal less to older generations.
This conference will explore the potential of national digital health strategies and systems that can offer cost effective solutions, harnessing the full power of information and communication technologies (ICT) for the prevention, treatment and management of non-communicable diseases to improve health outcomes. Discussion will include focus on how digital solutions can contribute at primary healthcare levels and through better integrated systems.
This meeting builds on earlier Wilton Park discussions including on ‘Reimagining global health: self-care interventions and implications for healthcare’, ‘Artificial intelligence and global health’ and a series on ‘Digital health in Africa: leadership and coordination’.